A New Standard in Menstrual Health
-
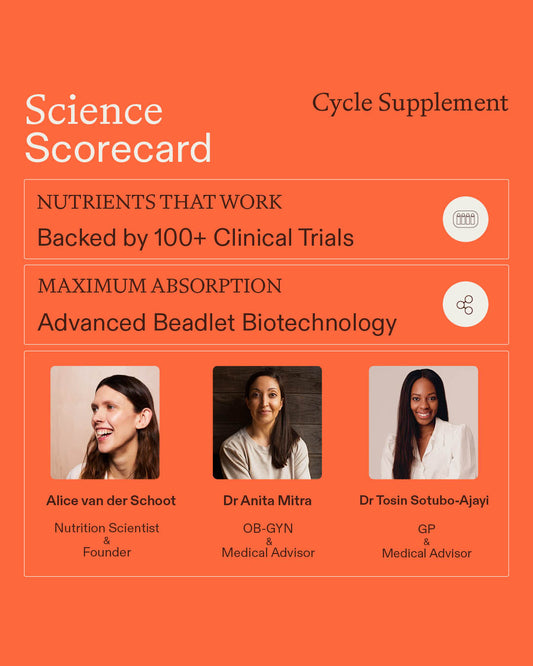
Formulated by scientists
-
Backed by 100+ clinical trials
-
Proactive daily support
-
Nutrient delivery biotechnology
Proven through Clinical Trials, Powered by Biotechnology
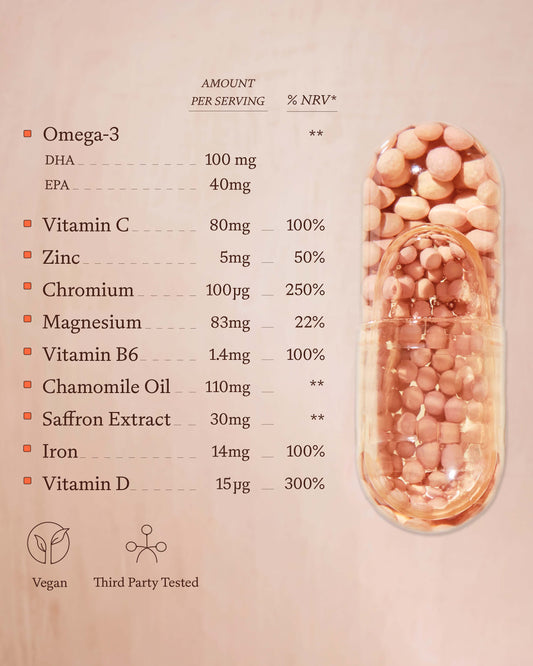
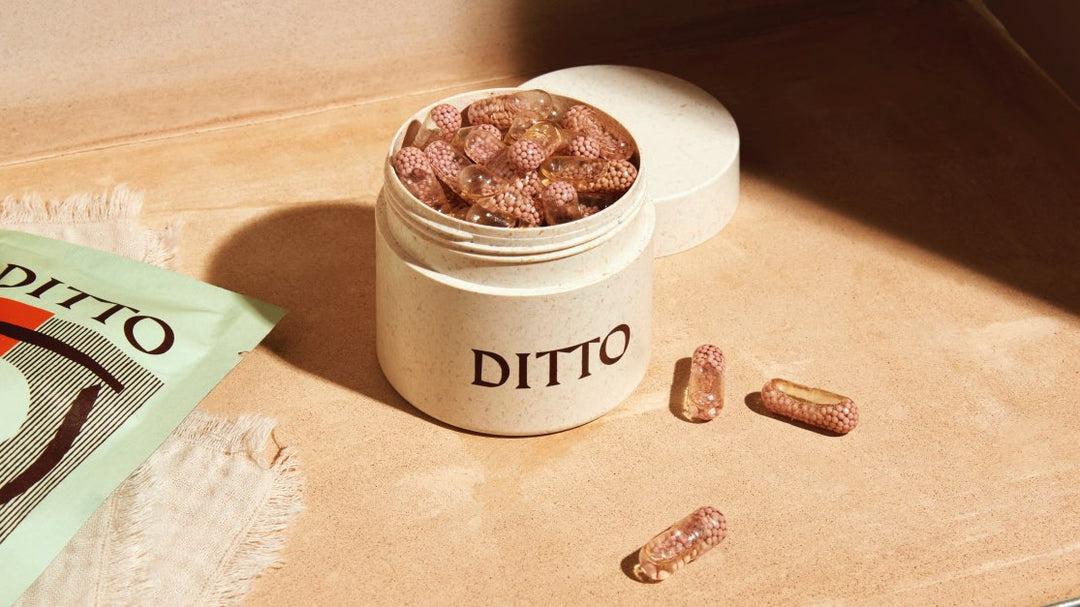
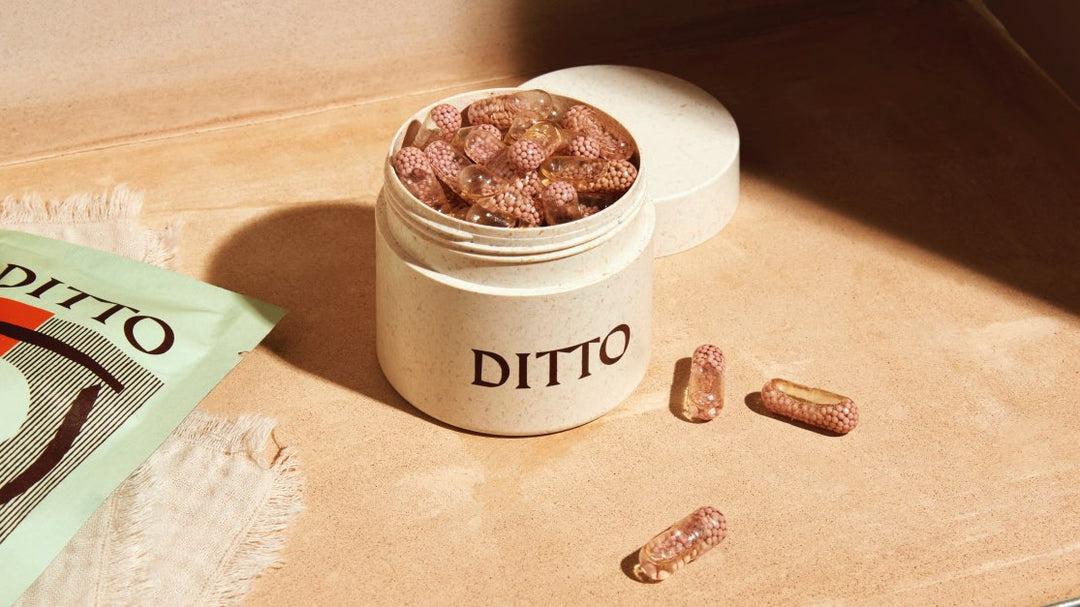
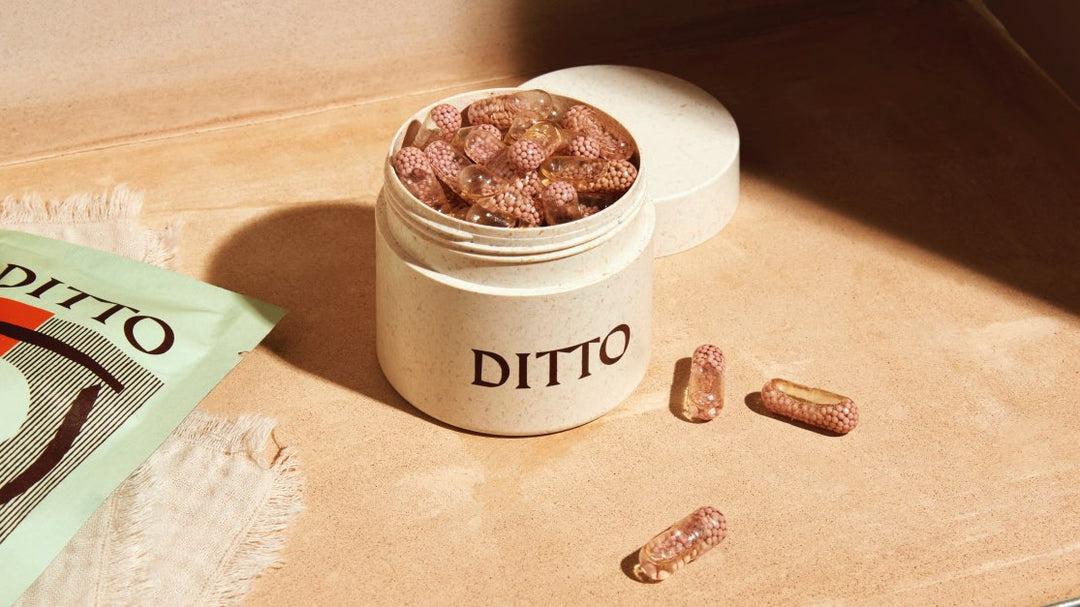
Cycle Supplement
- Reduces menstrual cycle symptoms.
- Formulated by women in science.
- 10 nutrients, 100+ clinical trials.
- Advanced nutrient biotechnology.
- For anyone with cycle symptoms.
- Also suitable if on contraception.
Clinical Trials: PMS, PMDD, PCOS, Endometriosis, Perimenopause
Vitamin D
Meta-analyses
- 11 studies: Lin KC, Huang KJ, Lin MN, Wang CY, Tsai TY. Vitamin D Supplementation for Patients with Dysmenorrhoea: A Meta-Analysis with Trial Sequential Analysis of Randomised Controlled Trials. Nutrients. 2024;16(7):1089
- 8 studies: Chen YC, Chiang YF, Lin YJ, et al. Effect of Vitamin D Supplementation on Primary Dysmenorrhea: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Nutrients. 2023;15(13):2830.
- 10 studies: Wang L, Wen X, Lv S, Tian S, Jiang Y, Yang X. Effects of vitamin D supplementation on metabolic parameters of women with polycystic ovary syndrome: a meta-analysis of randomized controlled trials. Gynecol Endocrinol. 2021;37(5):446-455.
- 9 studies: Fang F, Ni K, Cai Y, Shang J, Zhang X, Xiong C. Effect of vitamin D supplementation on polycystic ovary syndrome: A systematic review and meta-analysis of randomized controlled trials. Complement Ther Clin Pract. 2017;26:53-60.
Randomised placebo-controlled trials
- Moini A, Ebrahimi T, Shirzad N, et al. The effect of vitamin D on primary dysmenorrhea with vitamin D deficiency: a randomized double-blind controlled clinical trial. Gynecol Endocrinol. 2016;32(6):502-505.
- Rahnemaei FA, Gholamrezaei A, Afrakhteh M, et al. Vitamin D supplementation for primary dysmenorrhea: a double-blind, randomized, placebo-controlled trial. Obstet Gynecol Sci. 2021;64(4):353-363
- Heidari H, Amani R, Feizi A, Askari G, Kohan S, Tavasoli P. Vitamin D Supplementation for Premenstrual Syndrome-Related inflammation and antioxidant markers in students with vitamin D deficient: a randomized clinical trial. Sci Rep. 2019;9(1):14939.
- Amzajerdi A, Keshavarz M, Ghorbali E, Pezaro S, Sarvi F. The effect of vitamin D on the severity of dysmenorrhea and menstrual blood loss: a randomized clinical trial. BMC Womens Health. 2023;23(1):138.
- Lasco A, Catalano A, Benvenga S. Improvement of primary dysmenorrhea caused by a single oral dose of vitamin D: results of a randomized, double-blind, placebo-controlled study. Arch Intern Med. 2012;172(4):366-367.
- Ataee M, Zangeneh M, Mahboubi M. Cholecalciferol for primary dysmenorrhea in a college aged population—A clinical trial. J. Biol. Todays World. 2015;4:54–57.
- Behum. Coimbatore Medical College; Coimbatore, India: 2017. Study of Prevalence of Vitamin d Deficiency in Primary Dysmenorrhea and Administration of a Single Oral Dose of Vitamind to Improve Primary Dysmenorrhea. Master’s Thesis. 2017.
- Pakniat H, Chegini V, Ranjkesh F, Hosseini MA. Comparison of the effect of vitamin E, vitamin D and ginger on the severity of primary dysmenorrhea: a single-blind clinical trial. Obstet Gynecol Sci. 2019;62(6):462-468.
- Tartagni M, Cicinelli MV, Tartagni MV, et al. Vitamin D Supplementation for Premenstrual Syndrome-Related Mood Disorders in Adolescents with Severe Hypovitaminosis D. J Pediatr Adolesc Gynecol. 2016;29(4):357-361
- Mehdizadehkashi A, Rokhgireh S, Tahermanesh K, Eslahi N, Minaeian S, Samimi M. The effect of vitamin D supplementation on clinical symptoms and metabolic profiles in patients with endometriosis. Gynecol Endocrinol. 2021;37(7):640-645.
- Hajhashemi M, Ansari M, Haghollahi F, Eslami B. The effect of vitamin D supplementation on the size of uterine leiomyoma in women with vitamin D deficiency. Caspian J Intern Med. 2019;10(2):125-131.
Case-control and cross-sectional studies
Associations between low vitamin D and menstrual cycle symptoms
- Bertone-Johnson ER, Hankinson SE, Bendich A, Johnson SR, Willett WC, Manson JE. Calcium and vitamin D intake and risk of incident premenstrual syndrome. Arch Intern Med. 2005;165(11):1246-1252
- Jarosz AC, El-Sohemy A. Association between Vitamin D Status and Premenstrual Symptoms. J Acad Nutr Diet. 2019;119(1):115-123.
- Zeynali M, Haghighian HK. Is there a relationship between serum vitamin D with dysmenorrhea pain in young women?. J Gynecol Obstet Hum Reprod. 2019;48(9):711-714.
Zinc
Meta-analyses
- 6 studies: Hsu TJ, Hsieh RH, Huang CH, et al. Efficacy of Zinc Supplementation in the Management of Primary Dysmenorrhea: A Systematic Review and Meta-Analysis. Nutrients. 2024;16(23):4116.
Randomised placebo-controlled trials
- Jafari F, Amani R, Tarrahi MJ. Effect of Zinc Supplementation on Physical and Psychological Symptoms, Biomarkers of Inflammation, Oxidative Stress, and Brain-Derived Neurotrophic Factor in Young Women with Premenstrual Syndrome: a Randomized, Double-Blind, Placebo-Controlled Trial. Biol Trace Elem Res. 2020;194(1):89-95.
- Obiagwu HI, Eleje GU, Obiechina NJA, et al. Efficacy of zinc supplementation for the treatment of dysmenorrhoea: a double-blind randomised controlled trial. J Int Med Res. 2023;51(5):3000605231171489.
- Zekavat OR, Karimi MY, Amanat A, Alipour F. A randomised controlled trial of oral zinc sulphate for primary dysmenorrhoea in adolescent females. Aust N Z J Obstet Gynaecol. 2015;55(4):369-373.
- Siahbazi S, Behboudi-Gandevani S, Moghaddam-Banaem L, Montazeri A. Effect of zinc sulfate supplementation on premenstrual syndrome and health-related quality of life: Clinical randomized controlled trial. J Obstet Gynaecol Res. 2017;43(5):887-894.
- Ahmadi M, Khansary S, Parsapour H, Alizamir A, Pirdehghan A. The Effect of Zinc Supplementation on the Improvement of Premenstrual Symptoms in Female University Students: a Randomized Clinical Trial Study. Biol Trace Elem Res. 2023;201(2):559-566.
- Kashefi F, Khajehei M, Tabatabaeichehr M, Alavinia M, Asili J. Comparison of the effect of ginger and zinc sulfate on primary dysmenorrhea: a placebo-controlled randomized trial. Pain Manag Nurs. 2014;15(4):826-833.
- Sangestani G, Khatibanv M, Marci R, Piva I. The Positive Effects of Zinc Supplements on the Improvement of Primary Dysmenorrhea and Premenstrual Symptoms: A Double-blind, Randomized, Controlled Trial. Journal of Midwifery and Reproductive Health. 2015. 3(3), 378-384.
- Teimoori B, Ghasemi M, Hoseini ZS, Razavi M. The Efficacy of Zinc Administration in the Treatment of Primary Dysmenorrhea. Oman Med J. 2016;31(2):107-111.
- Safdar F., Kalsoom S., Majeed N., Nisa K., Riaz M., Tariq S. Comparison of Efficacy and Safety of Zinc Gluconate versus Placebo for Treatment of Primary Dysmenorrhea. J. Rawalpindi Med. Coll. 2022;26:363–367.
- Obiagwu HI, Eleje GU, Obiechina NJA, et al. Efficacy of zinc supplementation for the treatment of dysmenorrhoea: a double-blind randomised controlled trial. J Int Med Res. 2023;51(5):3000605231171489.
- Afshar Ebrahimi F, Foroozanfard F, Aghadavod E, Bahmani F, Asemi Z. The Effects of Magnesium and Zinc Co-Supplementation on Biomarkers of Inflammation and Oxidative Stress, and Gene Expression Related to Inflammation in Polycystic Ovary Syndrome: a Randomized Controlled Clinical Trial. Biol Trace Elem Res. 2018;184(2):300-307.
- Jamilian M, Foroozanfard F, Bahmani F, Talaee R, Monavari M, Asemi Z. Effects of Zinc Supplementation on Endocrine Outcomes in Women with Polycystic Ovary Syndrome: a Randomized, Double-Blind, Placebo-Controlled Trial. Biol Trace Elem Res. 2016;170(2):271-278.
Case-control studies
Associations between low zinc & menstrual cycle symptoms
- Fathizadeh S, Amani R, Haghighizadeh MH, Hormozi R. Comparison of serum zinc concentrations and body antioxidant status between young women with premenstrual syndrome and normal controls: A case-control study [published correction appears in Int J Reprod Biomed. Int J Reprod Biomed. 2016;14(11):699-704.
- Chocano-Bedoya PO, Manson JE, Hankinson SE, et al. Intake of selected minerals and risk of premenstrual syndrome. Am J Epidemiol. 2013;177(10):1118-1127.
Omega-3
Meta-analyses
- 8 studies: Mohammadi MM, Dehghan Nayeri N, Mashhadi M, Varaei S. Effect of omega-3 fatty acids on premenstrual syndrome: A systematic review and meta-analysis. J Obstet Gynaecol Res. 2022;48(6):1293-1305
- 8 studies: Snipe RMJ, Brelis B, Kappas C, et al. Omega-3 long chain polyunsaturated fatty acids as a potential treatment for reducing dysmenorrhoea pain: Systematic literature review and meta-analysis. Nutr Diet. 2024;81(1):94-106.
- 10 studies: Xia Y, Wang Y, Cui M, Su D. Efficacy of omega-3 fatty acid supplementation on cardiovascular risk factors in patients with polycystic ovary syndrome: a systematic review and meta-analysis. Ann Palliat Med. 2021;10(6):6425-6437.
- 9 studies: Yang K, Zeng L, Bao T, Ge J. Effectiveness of Omega-3 fatty acid for polycystic ovary syndrome: a systematic review and meta-analysis. Reprod Biol Endocrinol. 2018;16(1):27.
Randomised placebo-controlled trials
- Rocha Filho EA, Lima JC, Pinho Neto JS, Montarroyos U. Essential fatty acids for premenstrual syndrome and their effect on prolactin and total cholesterol levels: a randomized, double blind, placebo-controlled study. Reprod Health. 2011;8:2.
- Mano Y, Kato A, Fukuda N, Yamada K, Yanagimoto K. Influence of Ingestion of Eicosapentaenoic Acid-Rich Fish Oil on Oxidative Stress at the Menstrual Phase: A Randomized, Double-Blind, Placebo-Controlled, Parallel-Group Trial. Womens Health Rep (New Rochelle). 2022;3(1):643-651.
- Sohrabi N, Kashanian M, Ghafoori SS, Malakouti SK. Evalua-tion of the effect of omega-3 fatty acids in the treatment of pre-menstrual syndrome: “a pilot trial”. Complement Ther Med.2013;21(3):141–6
- Tofighiyan T, Kooshki A, Hassan RM. The effects of omega-3 fatty acids on premenstrual syndrome. Iran J Obstet Gynecol Infertil. 2013; 15(32): 23–8.
- Abbasinia K, Hosini F. A comparative study of the effects of Omega-3 and Perforan on severity mood symptoms in pre-menstrual syndrome. Complement Med J. 2013;3(3):529–40
- Jamilian M, Jamilian H, Mirzaie S. Rose Damascenavs. Omega-3 in the treatment of premenstural syndrome: Arandomized, and placebo-controlled clinical trial. Comple-ment Med J. 2013;3(3):541–51.
- Behboudi-Gandevani S, Hariri FZ, Moghaddam-Banaem L.The effect of omega 3 fatty acid supplementation on premen-strual syndrome and health-related quality of life: a random-ized clinical trial. J Psychosom Obstet Gynaecol. 2018;39(4):266–72
- Sadeghi N, Paknezhad F, Rashidi Nooshabadi M, Kavianpour M, Jafari Rad S, Khadem Haghighian H. Vitamin E and fish oil, separately or in combination, on treatment of primary dysmenorrhea: a double-blind, randomized clinical trial. Gynecol Endocrinol. 2018;34(9):804-808.
- Deutch B, Jørgensen EB, Hansen JC. Menstrual discomfort in Danish women reduced by dietary supplements of omega-3 PUFA and B12 (fish oil or sea oil capsules). Nutr Res. 2000; 20(5):621-631.
- Mandana Z, Azar A. Comparison of the effect of vit E, vitB6,calcium and omega-3 on the treatment of premenstrual syn-drome: a clinical randomized trial. Ann Res Rev Biol. 2014;4:1141–9
- Kheirkhah M, Gholami R, Ghare-shiran SY, Abbasinia H.Comparison of the effect of omega-3 fatty acids andperforan (Hypericum perforatum) on severity of premen-strual syndrome (PMS): a randomized trial. Int J Med ResHealth Sci. 2016;5(11):333–40
- Harel Z, Biro FM, Kottenhahn RK, Rosenthal SL. Supplementation with omega-3 polyunsaturated fatty acids in the management of dysmenorrhea in adolescents. Am J Obstet Gynecol. 1996;174(4):1335-1338.
- Moghadamnia AA, Mirhosseini N, Abadi MH, Omranirad A, Omidvar S. Effect of Clupeonella grimmi (anchovy/kilka) fish oil on dysmenorrhoea. East Mediterr Health J. 2010;16(4):408-413
Saffron
Randomised placebo-controlled trials
- Rajabi F, Rahimi M, Sharbafchizadeh MR, Tarrahi MJ. Saffron for the Management of Premenstrual Dysphoric Disorder: A Randomized Controlled Trial. Adv Biomed Res. 2020;9:60.
- Agha-Hosseini M, Kashani L, Aleyaseen A, et al. Crocus sativus L. (saffron) in the treatment of premenstrual syndrome: a double-blind, randomised and placebo-controlled trial. BJOG. 2008;115(4):515-519.
- Beiranvand S, Beiranvand N, Moghadam Z, Birjandi M, Azhari S, Rezaei E, et al. The effect of crocus sativus (saffron) on the severity of premenstrual syndrome. Eur J Integr Med. 2016;8(1):55-61.
Chamomile
Randomised placebo-controlled trials
- Najafi Mollabashi E, Ziaie T, Bostani Khalesi Z. The effect of Matricaria chamomile on menstrual related mood disorders. Eur J Obstet Gynecol Reprod Biol X. 2021;12:100134.
- Saghafi N, Rhkhshandeh H, Pourmoghadam N, et al. Effectiveness of Matricaria chamomilla (chamomile) extract on pain control of cyclic mastalgia: a double-blind randomised controlled trial. J Obstet Gynaecol. 2018;38(1):81-84.
- Khalajinia Z, Falahieh FM, Aghaali M. The Effects of Chamomile and Flaxseed on Pelvic Pain, Dyspareunia, and Dysmenorrhea in Endometriosis: A Controlled Randomized Clinical Trial. Iran J Nurs Midwifery Res. 2024;29(6):731-736
Systematic reviews
- 8 studies: Khalesi ZB, Beiranvand SP, Bokaie M. Efficacy of Chamomile in the Treatment of Premenstrual Syndrome: A Systematic Review. J Pharmacopuncture. 2019;22(4):204-209
- 8 studies: Niazi A, Moradi M. The Effect of Chamomile on Pain and Menstrual Bleeding in Primary Dysmenorrhea: A Systematic Review. Int J Community Based Nurs Midwifery. 2021;9(3):174-186
Iron
Randomised placebo-controlled trials
- Vaucher P, Druais PL, Waldvogel S, Favrat B. Effect of iron supplementation on fatigue in nonanemic menstruating women with low ferritin: a randomized controlled trial. CMAJ. 2012;184(11):1247-1254.
- Verdon F, Burnand B, Stubi CL, et al. Iron supplementation for unexplained fatigue in non-anaemic women: double blind randomised placebo controlled trial. BMJ. 2003;326(7399):1124.
Case-control studies
Associations between low iron and menstrual cycle symptoms
- Chocano-Bedoya PO, Manson JE, Hankinson SE, et al. Intake of selected minerals and risk of premenstrual syndrome. Am J Epidemiol. 2013;177(10):1118-1127.
Vitamin C (increases iron absorption)
- Heffernan A, Evans C, Holmes M, Moore JB. The Regulation of Dietary Iron Bioavailability by Vitamin C: A Systematic Review and Meta-Analysis. Proceedings of the Nutrition Society. 2017;76(OCE4):E182.
Health Claims
Non-haem iron absorption
- European Food Safety Authority (EFSA) - Vitamin C related Health Claims. https://www.efsa.europa.eu/en/efsajournal/pub/1226
Magnesium
Randomised placebo-controlled trials
- Yaralizadeh M, Nezamivand-Chegini D , Najar S , Namjoyan F , Abedi . Effectiveness of magnesium on menstrual symptoms among dysmenorrheal college students: A randomized controlled trial. International Journal of Women's Health & Reproduction Sciences. 2024. 12(2).
- Fathizadeh N, Ebrahimi E, Valiani M, Tavakoli N, Yar MH. Evaluating the effect of magnesium and magnesium plus vitamin B6 supplement on the severity of premenstrual syndrome. Iran J Nurs Midwifery Res. 2010;15(Suppl 1):401-405.
- Walker AF, De Souza MC, Vickers MF, Abeyasekera S, Collins ML, Trinca LA. Magnesium supplementation alleviates premenstrual symptoms of fluid retention. J Womens Health. 1998;7(9):1157-1165.
- Facchinetti F, Sances G, Borella P, Genazzani AR, Nappi G. Magnesium prophylaxis of menstrual migraine: effects on intracellular magnesium. Headache. 1991;31(5):298-301. doi:10.1111/j.1526-4610.1991.hed3105298.x
- De Souza MC, Walker AF, Robinson PA, Bolland K. A synergistic effect of a daily supplement for 1 month of 200 mg magnesium plus 50 mg vitamin B6 for the relief of anxiety-related premenstrual symptoms: a randomized, double-blind, crossover study. J Womens Health Gend Based Med. 2000;9(2):131-139
- Facchinetti F, Borella P, Sances G, Fioroni L, Nappi RE, Genazzani AR. Oral magnesium successfully relieves premenstrual mood changes. Obstet Gynecol. 1991;78(2):177-181.
- Seifert B, Wagler P, Dartsch S, Schmidt U, Nieder J. Magnesium--eine therapeutische Alternative bei der primären Dysmenorrhoe [Magnesium--a new therapeutic alternative in primary dysmenorrhea]. Zentralbl Gynakol. 1989;111(11):755-760.
- De Souza MC, Walker AF, Robinson PA, Bolland K. A synergistic effect of a daily supplement for 1 month of 200 mg magnesium plus 50 mg vitamin B6 for the relief of anxiety-related premenstrual symptoms: a randomized, double-blind, crossover study. J Womens Health Gend Based Med. 2000;9(2):131-139.
- Afshar Ebrahimi F, Foroozanfard F, Aghadavod E, Bahmani F, Asemi Z. The Effects of Magnesium and Zinc Co-Supplementation on Biomarkers of Inflammation and Oxidative Stress, and Gene Expression Related to Inflammation in Polycystic Ovary Syndrome: a Randomized Controlled Clinical Trial. Biol Trace Elem Res. 2018;184(2):300-307.
- Jaripur M, Ghasemi-Tehrani H, Askari G, Gholizadeh-Moghaddam M, Clark CCT, Rouhani MH. The effects of magnesium supplementation on abnormal uterine bleeding, alopecia, quality of life, and acne in women with polycystic ovary syndrome: a randomized clinical trial. Reprod Biol Endocrinol. 2022;20(1):110.
- Shahmoradi S, Chiti H, Tavakolizadeh M, Hatami R, Motamed N, Ghaemi M. The Effect of Magnesium Supplementation on Insulin Resistance and Metabolic Profiles in Women with Polycystic Ovary Syndrome: a Randomized Clinical Trial [published correction appears in Biol Trace Elem Res. 2024 May;202(5):2402.
Vitamin B6
Randomised placebo-controlled trials
- Randabunga, Ervan & Lukas, Efendi & Tumedia, Josephine & Chalid, Maisuri. (2018). Effect of Pyridoxine on Prostaglandin Plasma Level for Primary Dysmenorrheal Treatment. Indonesian Journal of Obstetrics and Gynecology. 239. 10.32771/inajog.v6i4.848
- De Souza MC, Walker AF, Robinson PA, Bolland K. A synergistic effect of a daily supplement for 1 month of 200 mg magnesium plus 50 mg vitamin B6 for the relief of anxiety-related premenstrual symptoms: a randomized, double-blind, crossover study. J Womens Health Gend Based Med. 2000;9(2):131-139.
- Fathizadeh N, Ebrahimi E, Valiani M, Tavakoli N, Yar MH. Evaluating the effect of magnesium and magnesium plus vitamin B6 supplement on the severity of premenstrual syndrome. Iran J Nurs Midwifery Res. 2010;15(Suppl 1):401-405.
- Williams MJ, Harris RI, Dean BC. Controlled trial of pyridoxine in the premenstrual syndrome. J Int Med Res. 1985;13(3):174-179.
- Kashanian M, Mazinani R, Jalalmanesh S, Babayanzad Ahari S. Pyridoxine (vitamin B6) therapy for premenstrual syndrome. Int J Gynaecol Obstet. 2007;96(1):43-44.
- Wyatt KM, Dimmock PW, Jones PW, Shaughn O'Brien PM. Efficacy of vitamin B-6 in the treatment of premenstrual syndrome: systematic review. BMJ. 1999;318(7195):1375-1381.
- Ebrahimi E, Khayati Motlagh S, Nemati S, Tavakoli Z. Effects of magnesium and vitamin b6 on the severity of premenstrual syndrome symptoms. J Caring Sci. 2012;1(4):183-189.
Systematic review
- 9 studies: Wyatt KM, Dimmock PW, Jones PW, Shaughn O’Brien PM. Efficacy of vitamin B-6 in the treatment of premenstrual syndrome: systematic review. BMJ 1999;318:1375-81
Chromium
Randomised placebo-controlled trials
- Anton SD, Morrison CD, Cefalu WT, et al. Effects of chromium picolinate on food intake and satiety. Diabetes Technol Ther. 2008;10(5):405-412.
- Lucidi RS, Thyer AC, Easton CA, Holden AE, Schenken RS, Brzyski RG. Effect of chromium supplementation on insulin resistance and ovarian and menstrual cyclicity in women with polycystic ovary syndrome. Fertil Steril. 2005;84(6):1755-1757.
- Jamilian M, Asemi Z. Chromium Supplementation and the Effects on Metabolic Status in Women with Polycystic Ovary Syndrome: A Randomized, Double-Blind, Placebo-Controlled Trial. Ann Nutr Metab. 2015;67(1):42-48. doi:10.1159/000438465
- Ashoush S, Abou-Gamrah A, Bayoumy H, Othman N. Chromium picolinate reduces insulin resistance in polycystic ovary syndrome: Randomized controlled trial. J Obstet Gynaecol Res. 2016;42(3):279-285
Health Claims
Contribution to normal macronutrient metabolism, maintenance of normal blood glucose concentrations, contribution to the maintenance or achievement of a normal body weight.
- European Food Safety Authority (EFSA) Journal - Chromium Related Health Claims. https://www.efsa.europa.eu/en/efsajournal/pub/1732
-
Cravings
-
Cramps
-
Fatigue
-
Mood
-
Bloating
-
Breast Tenderness
-
Headaches
-
Anxiety

-
Irritability

- Vegan
- Gluten-free
- Dairy-free
- Non-GMO
- Sugar-free
- Third party tested
Formulated by leading female scientists
Formulated by leading female scientists
Alice specialises in evidence-based nutrition, laboratory work and clinical trials. With a strong dedication to the highest standards of science, she translates clinical trial findings into effective solutions for her DITTO community.
Dr. Anita Mitra is a gynaecologist with 10+ years NHS experience, specialising in surgery for gynaecological cancers and treating conditions like fibroids, PCOS, and endometriosis. Known online as 'The Gynae Geek' (also the title of her first book), she is the author of Dealing with Problem Periods. She holds a PhD from Imperial College London.
Dr Tosin brings over a decade of clinical experience across the NHS and private health sector, with a particular focus in Women’s Health. She has been featured in a number of publications and is an advisory mentor for FemTech Lab.
Trusted by people like you



















Science that tells us it will work for you.
We’ve carefully selected our nutrients from studies that are randomised, placebo-controlled and conducted in people with cycle symptoms.
Our daily capsules transcend the traditional reactive model of only addressing symptoms during menstruation. They proactively support our cycles.

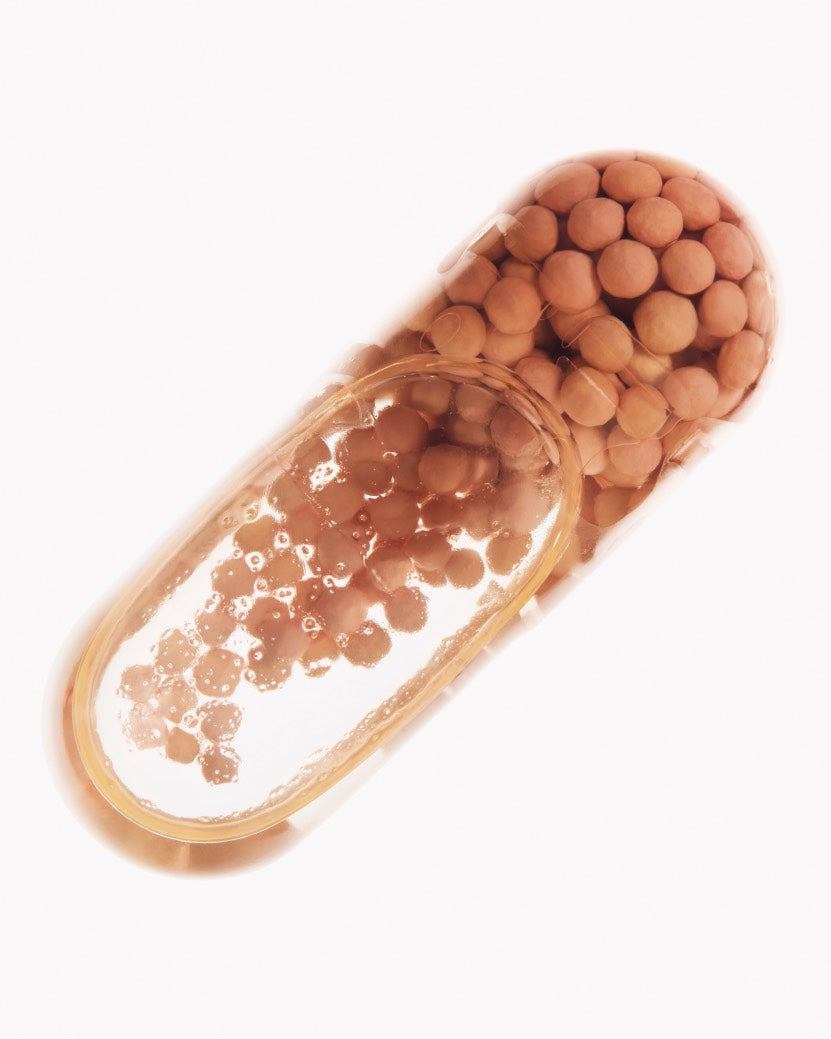
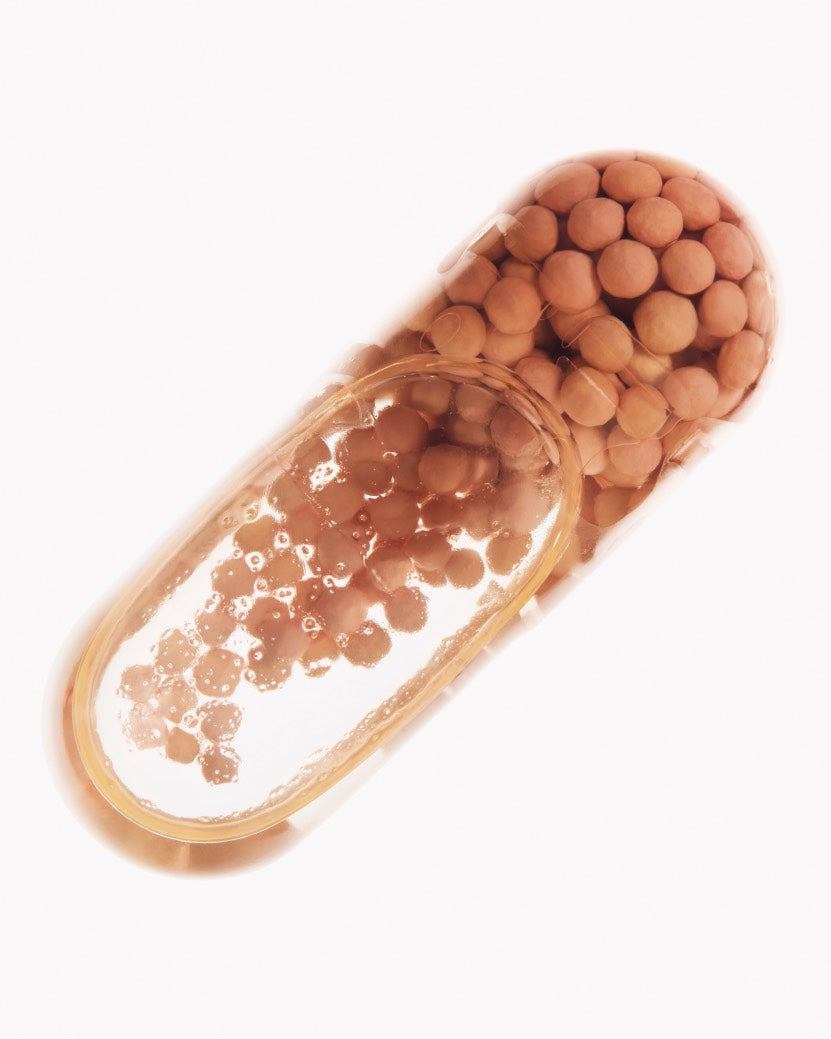
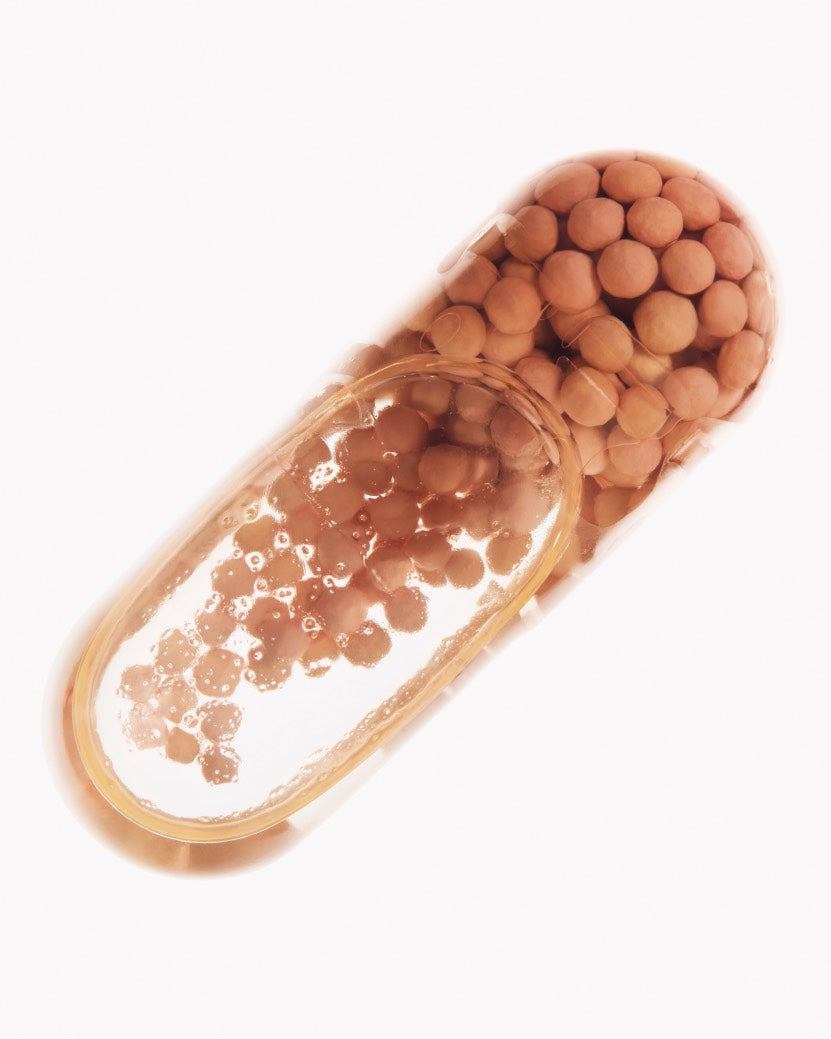
Nutrient Delivery Biotechnology
Did you know? In standard supplements, when nutrients are released all at once, they can actually block each other's absorption.
Engineered for Maximum Absorption
The technology allows timed and targeted release of different nutrients, reducing interference.
Developed for Steady Release
The beadlets gradually release their contents.
Kind to your Body
Infused with citrus flavour and gentle on your gut, taking the capsules is an enjoyable experience.
Simplified Routine
It combines oil and dry ingredients, meaning that you no longer need multiple supplements.
Menstrual Health Research
Breaking the taboo, empowering the conversation, and bringing menstrual health research to everyone.
Your Cycle, Your Way
-
FREE SHIPPING
Across all subscriptions
-
FLEXIBLE PLAN
Skip, pause or cancel anytime
-
REFERRALS
Give 20%, get 20% on referrals
-
RISK-FREE
30 day money-back guarantee